LCFA believes
Research
makes living with lung cancer possible
New discoveries in lung cancer research, such as LCFA-funded research, result in new treatments for lung cancer patients.
Because of research, the survival rate for lung cancer rate has doubled.
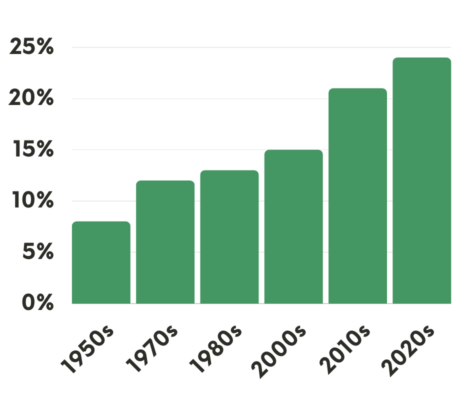
Improvement of the 5-year Survival Rate for Lung Cancer
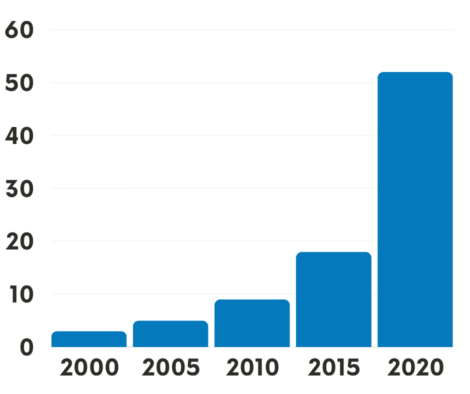
# of FDA-approved Treatments for Lung Cancer over the past 20 years
Learn about these 5 Exciting Areas of Lung Cancer Research
Treatments that target specific biomarkers that are present in lung cancer tumors continue to have great success, especially in treating patients with:
It is recommended that all patients get comprehensive biomarker testing when they are first diagnosed. A biomarker is a feature of the cancer that can help determine a personalized treatment. It is advisable for patients to discuss with their doctors how and when to schedule a complete panel of biomarker testing. This is preferably before any treatment is started. Comprehensive biomarker testing, specified in the NCCN guidelines, will provide the most complete assessment. This assessment can help to determine the most effective treatment plan.
Immunotherapy is another very effective treatment option that uses the body’s own immune response to fight the cancer without damaging healthy cells. In the past few years, lung cancer research has yielded new medications that can be used to stop cancer cells from being able to turn off the immune system. This allows it to do its work in battling the cancer.
In addition, various forms of liquid biopsy are being studied that can identify molecular abnormalities of lung cancer without the need for invasive procedures. These specialized blood tests make use of readily accessible specimens like blood, saliva, or even exhaled breath.
Lung cancer research has rapidly advanced robotics used in surgeries, which allow for quicker recovery for lung cancer patients who have tumors resected. Board certified thoracic surgeons are able to remove the cancerous tissue with minimally invasive techniques, which allow for far smaller incision sites and more rapid recovery for patients.
Stereotactic radiation is a type of external radiation therapy that uses special equipment to position the patient and precisely deliver radiation to a tumor. Advances in techniques using stereotactic radiation allow for effective treatment of brain metastases.
LCFA Funds Impactful Young Investigator Research Grants
“Based on my own personal experience, the LCFA Young Investigator award was the very first grant that I was ever awarded. I’ve been able to leverage that now into several million dollars worth of funding.”
~Dr. Kellie Smith, assistant professor of oncology at Johns Hopkins Medicine
Meet the Researchers
All Researchers-
Aparna Sharma, DM
Thoracic medical oncologist
Genomic characterization of young onset lung adenocarcinoma

-
Julie Wu, MD
Staff Physician, Medical Oncology
Precision oncology integrating evidence-based models into clinical practice to personalize treatment approaches

-
Jonathan Villena-Vargas, MD
Thoracic Surgeon
Characterizing T cell PD-1 response in the tumor-draining lymph nodes of early-stage NSCLC patients

New discoveries in lung cancer are happening at a rapid pace.
Join our community to get the latest new on lung cancer research.