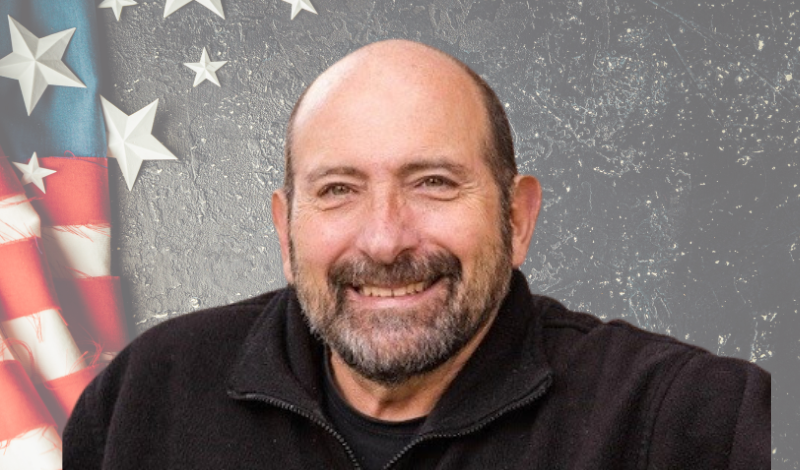
Jim Pantelas’s lung cancer journey began nearly twenty years ago. Yes, twenty years ago. An incidental finding, the symptoms of which were atypical for lung cancer, led to the shocking discovery.
Vietnam Era Vet Exposed To Carcinogens During His Service
Jim served in the Navy in the Vietnam War era. As he says, “In my era, Agent Orange was a given.” According to the Journal of Thoracic and Cardiovascular Surgery, Agent Orange, one of the tactical herbicides used by the armed forces as a means of destroying crops and clearing vegetation, has been linked to the development of several cancers including non–small cell lung cancer. Jim’s lung cancer wasn’t deemed to be a result of his time serving in the Navy at first, but over the years that has changed. The fact that Jim’s service included working in large computer installations in rooms protected by asbestos (a known risk for lung cancer) indicates that his years in the Navy at least contributed to his diagnosis.
About his work as a lung cancer advocate, Jim says, “We are service driven. And it is about the next guy. I mean, you don’t get people functioning in a war zone because they want to be there. You get them functioning in the war zone because they want to make sure somebody else doesn’t have to.”
That attitude has carried forward into Jim’s life after his service. LCFA is grateful to have him as a member of our Veterans Speakers Bureau.
A New Century And A New Life For Jim
In 2000, Jim had restarted his life. He was divorced and was seriously contemplating retiring and heading south to Naples, Florida. His move took a backseat, not because of his lung cancer diagnosis, though. Jim met a wonderful woman whom he married two years later, in 2002. Together they began a life, including the purchase of a new home. Jim recalls a day that he and his father-in-law were working together to finish the basement of the house:
“I was exhausted. Not an I’ve-been-working tired, but rather a complete body exhaustion. At first, I thought it might be related to a recent change in cholesterol-lowering medication, but, even after my doctor adjusted it, I was not only growing even more exhausted more quickly, but my joints started to hurt enough so that I went to see a rheumatologist. About 45 minutes into the conversation he mentioned, very matter-of-factly, that I had a tumor in my lung. That discovery helped to explain the bone pain: my body was taking away oxygen from where it was least needed, which impacted my bones, making them brittle and painful.”
This was a shocking piece of news.
A Lung Cancer Diagnosis for This Vietnam Era Vet
Jim, his head spinning with this information, went to see his primary care physician. He had a chest x-ray and a CAT scan which revealed a 3 cm tumor in his right lung which had spread to his lymph nodes. As luck would have it, he was at a large hospital that boasted a multidisciplinary cancer clinic far more advanced than most hospitals. There, he met with a team of physicians: a thoracic surgeon, a radiation oncologist, a head oncologist, and a pain management nurse practitioner. The team determined that his lung cancer was stage 1b. Just days later, Jim would undergo a lobectomy removing ¾ of his right lung. It was during that procedure that the medical team discovered that the disease had spread to the farthest excised lymph node. He would awaken from surgery only to be told that his lung cancer was, in actuality, Stage 3b. It was 2005 and at that time the survival rate for Jim’s non-small cell adenocarcinoma diagnosis was grim: two-year survival was less than 1%.
A dire diagnosis for anyone but for Jim it was especially horrendous: his wife was 6 and a half months pregnant with their first child.
Jim was ready to do whatever he had to do. He underwent aggressive chemotherapy and radiation which, at the time, was the only treatment option available. Today, thanks to research, including biomarker testing, medications are far more targeted and less difficult to tolerate. At the time, the only medication available to alleviate the symptoms of the treatments was opioids. With a baby on the way, he refused to take them, choosing his pain over an inability to care for his wife and baby.
Vietnam Era Vet Survives Lung Cancer Energized by New Baby
When his daughter Stella was born, Jim was two rounds into treatment. Her birth energized him to keep fighting. And then, another unexpected curveball: at just 21 days old, Stella began having seizures and suffered a brain bleed. The cause was quickly determined to be meningitis. And, to make a devastating situation even worse, it was nearly impossible to find a hospital NICU that would admit her for treatment; she was considered a “dirty baby” having been out in the world, which could be dangerous to other newborns in the hospital. This was an extraordinarily difficult time. While her birth hospital could not admit Stella to their NICU, a hospital across town did and, there, she received life-saving care.
“Things pile up and you can take the “why am I being punished” route or you can just get up and deal with it. I am not religious, but I do believe in a loving God. God gives us free will over how we live and how we die…he didn’t put anything on my plate, this is my body’s experience and what I have to live with, and I live as fully as I can.
Not long after all of this started the furnace in the house went out. It was the dead of winter. I was strapped financially and things just kept piling on. But, and this is a big but, each of the issues we were dealing with served as a distraction from the others. Because of my cancer treatments, I was not able to work which, ironically, allowed me to spend time in the NICU with my daughter and wife. For that reason, and In a strange way, my lung cancer diagnosis was a blessing.”
Before his diagnosis, Jim seldom went to the doctor. As a result, he acknowledges knowing nothing about medicine, healthcare, hospitals, and what he aptly describes as the financial toxicity of being a patient. Suddenly, he needed to understand, navigate, manage, and advocate for himself and his daughter.
Seeking comfort and meaning during their medical crises, Jim’s wife Cathy started volunteering at the hospital overseeing Stella’s care. At the time, the hospital was launching a new program whose goal was to look at both patient satisfaction and involvement. As a patient himself, Jim recognized the importance of this initiative and decided to also get involved, initially concerning pediatric ethics. He learned that hospitals all have Institutional Review Boards (IRB) which are tasked with overseeing ethics in a research setting. His involvement as an advocate for his daughter, who is now 18 years old, led him to the cancer IRB. To this day he remains actively involved.
Vietnam ERA Vet Survives Lung Cancer and Remains NED
Despite his grim diagnosis and short life expectancy, Jim has been NED (no evidence of disease) since 2006. Since that time, he has had two more daughters, Grace and Leda, He continues to undergo yearly scans and work tirelessly advocating for both pediatric and lung cancer patients.
“I was supposed to be dead. There have been a lot of I’ll be dead before this or I’ll be dead before that happens, but I just keep living. Two years ago I had an unrelated brain tumor and my youngest asked me if I was going to die. I promised her that I would do everything I could every day to live as long as I could. She asked for me to stick around until I am 112. I am going to try my best!”
I’m using my lungs to advocate
As a member of LCFA’s Speakers Bureau, I’m advocating for research and raising awareness through the media, embodying hope and action.
View Speaker Profile
